Introduction and History
Persistent Fetal Vasculature Syndrome (PFVS) is a rare eye condition present at birth. It occurs when certain blood vessels in the eye, which are supposed to disappear before birth, remain and cause problems. These blood vessels are part of the “primary vitreous” and are meant to nourish the developing eye in the womb. If they don’t regress as they should, they can lead to vision issues.
The condition was first clearly described in 1955 by an ophthalmologist named Dr. Algernon B. Reese, although he referred to it as “Persistent Hyperplastic Primary Vitreous” (PHPV). Dr. Morton F. Goldberg introduced the term “persistent fetal vasculature syndrome” as the condition’s new name in 1997. The preferred term is PFVS because it best describes the different ways the condition can appear.
Who Is Affected?
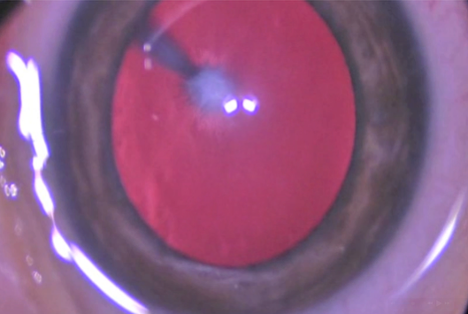
PFVS usually affects one eye (unilateral) but can sometimes affect both eyes (bilateral). It’s present at birth and is often noticed when a baby has a white spot in the eye (leukocoria). PFVS can occur in children with no other health problems, but in some cases, it may be linked to other conditions.
Diagnosis
Often, parents or a pediatrician might notice something unusual about the baby’s eye, such as:
An ophthalmologist, a specialist in eye care, will conduct a comprehensive eye exam. They might use special lights and magnifying tools to examine the inside of the eye. To get a better view of the back of the eye and the leftover vessels, they often use:
- Ultrasound: This uses sound waves to create a picture of the inside of the eye, much like an ultrasound for a pregnant mother.
- Sometimes, an MRI or CT scan may be used to obtain even more detailed images.
Treatment
The primary goal of treatment is to provide the child with the best possible vision and prevent other eye problems. Treatment depends on how severe the PFVS is:
- Observation: If the PFVS is mild and not causing major vision problems, the doctor might just monitor the eye closely.
- Surgical Treatment: If the PFVS is causing vision loss or could lead to complications like glaucoma (high eye pressure) or retinal detachment (where the light-sensitive layer at the back of the eye pulls away), surgery is often needed.
- The surgery usually involves carefully removing the leftover fetal blood vessels and any scar tissue.
- Sometimes, the eye’s natural lens, if cloudy (cataract), is also removed (this is called a lensectomy).
- The jelly-like substance inside the eye (the vitreous) might also be cleared (vitrectomy).
- Surgery is often done when the child is very young, usually within the first few months of life.
- Medical Treatment:
- After surgery, or even without it, children might need eye drops to reduce inflammation or control eye pressure.
- To help the vision develop in the affected eye, especially after surgery, children often need to wear an eye patch over their stronger eye for a few hours a day, a practice known as amblyopia therapy or “lazy eye” treatment.
- Glasses or contact lenses may also be needed.
Prognosis
The outlook for vision in a child with PFVS varies a lot. It depends on:
- How severe the PFVS was at the start.
- How much of the eye was affected?
- Whether other eye problems (like glaucoma or retinal detachment) develop.
- How early was the condition diagnosed and treated?
Some children can develop useful vision in the affected eye, especially with early surgery and dedicated follow-up care, including patching. However, even with the best treatment, some children may have permanent vision loss in the affected eye. Regular, lifelong check-ups with an eye doctor are very important.
Current Research
Researchers continually work to better understand PFVS and improve treatments. Current research focuses on:
- Finding the exact causes: Scientists are studying if there are genetic factors or specific events during pregnancy that might lead to PFVS.
- Improving surgical techniques: Doctors are refining surgical methods to make them safer and more effective, especially for very young babies.
- Better ways to manage complications: Research is ongoing to find more effective treatments for conditions like glaucoma that can occur with PFVS.
- Long-term outcomes: Studies are examining the growth and development of children with PFVS to inform and improve care strategies.
References
- Reese, A. B. (1955). Persistent hyperplastic primary vitreous. American Journal of Ophthalmology, 40(3), 317-331.
- Goldberg MF. Persistent fetal vasculature (PFV): an integrated interpretation of signs and symptoms associated with persistent hyperplastic primary vitreous (PHPV). LIV Edward Jackson Memorial Lecture. Am J Ophthalmol. 1997 Nov;124(5):587-626.
- De la Huerta I, Mesi O, Murphy B, Drenser KA, Capone A Jr, Trese MT. SPECTRAL DOMAIN OPTICAL COHERENCE TOMOGRAPHY IMAGING OF THE MACULA AND VITREOMACULAR INTERFACE IN PERSISTENT FETAL VASCULATURE SYNDROME WITH POSTERIOR INVOLVEMENT. Retina 2019 Mar;39(3):581-586.
- Walsh MK, Drenser KA, Capone A Jr, Trese MT. Early vitrectomy effective for bilateral combined anterior and posterior persistent fetal vasculature syndrome. 2010 Apr;30(4 Suppl):S2-8.