Congenital X-linked Retinoschisis
Introduction and History
Congenital X-Linked Retinoschisis, often referred to as XLRS, is a genetic eye condition that primarily affects males. It causes a splitting (the “schisis” part of the name) of the layers of the retina. The retina is the light-sensitive tissue at the back of your eye that acts like the film in a camera, capturing images and sending them to the brain.
When the retinal layers separate, small cysts or blisters may develop, particularly in the macula. The macula is the central part of the retina responsible for sharp, detailed vision, such as that used for reading or recognizing faces. This separation can harm the retina and result in blurry vision that typically cannot be fully corrected with glasses. Because it’s “X-linked,” it means the gene causing it is located on the X chromosome and is inherited from mothers (who are usually unaffected carriers) to their sons.
An ophthalmologist named Josef Haas first described this eye condition in young brothers in 1898, noticing the characteristic splitting of the retina in families.
Who Is Affected?
XLRS is a rare disorder that affects approximately 1 in every 5,000 to 25,000 males worldwide. Since the gene responsible for XLRS is located on the X chromosome, boys are primarily affected. Girls have two X chromosomes, which means that if one has the faulty gene, the other typically carries a healthy copy, and they usually do not exhibit symptoms (they are “carriers”). Symptoms often begin in early childhood, sometimes even during infancy, and are generally noticed when a child starts school and has difficulty seeing clearly.
Diagnosis
Doctors diagnose XLRS through a n eye doctor will examine the retina for tell-tale signs. The most common finding is a “spoke-wheel” pattern of cysts in the macula. About half of those with XLRS also have splitting in the peripheral (side) areas of the retina, resulting in a characteristic schisis cavity or “bulla” (Figure), sometimes creating “vitreous veils” (thin sheets floating in the gel inside the eye).
Optical Coherence Tomography (OCT) is a specialized scan that captures detailed cross-sectional images of the retina, clearly revealing the distinct layers and cysts. Electroretinogram (ERG): This test evaluates the electrical activity of the retina in response to light. In XLRS, there is often a characteristic pattern in which one type of electrical wave (the b-wave) is significantly smaller than normal. Genetic Testing: A blood or saliva test can identify changes (mutations) in the RS1 gene, which is responsible for XLRS. Family History: Because it’s inherited, knowing if other males in the family have experienced similar vision problems can be a clue.
Treatment
Currently, there is no cure for XLRS, and treatments aim to manage symptoms and complications:
Vision Correction: Glasses may be prescribed for nearsightedness or farsightedness, though they often don’t fully correct the blurry vision caused by the schisis. Patching may be used if one eye is weaker (amblyopia or “lazy eye”).
Carbonic Anhydrase Inhibitors (CAIs): These medications (eye drops like dorzolamide or pills like acetazolamide) can sometimes help reduce the fluid in the retinal cysts for some patients, but their effects can vary and may not lead to significant vision improvement for everyone.
Surgery: Surgery is typically reserved for serious complications. If the retina detaches (pulls away completely from the back of the eye) or if there is significant bleeding into the vitreous (the gel filling the eye), an eye surgeon may perform procedures such as a vitrectomy (removing the vitreous gel) or a scleral buckle (placing a supporting band around the eye). Regular eye check-ups are very important for monitoring the condition and catching any complications early.
Prognosis
The course of XLRS can vary a lot, even within the same family. Vision often gets worse during childhood and teenage years but then may stay stable for many years in adulthood. However, some people can experience a further decline in vision later in life, especially in their 50s or 60s, or if complications like retinal detachment occur.
Most people with XLRS maintain useful vision, especially peripheral vision. Central vision is variably affected. Complete blindness is rare but can happen with severe complications.
Current Research
There is a lot of exciting research taking place to discover better treatments for XLRS, with a major focus on gene therapy. The aim of gene therapy is to deliver a healthy copy of the RS1 gene directly into retinal cells using a harmless modified virus, often an adeno-associated virus (AAV), as the delivery vehicle. Several clinical trials for gene therapy in XLRS have occurred or are currently ongoing. For instance, a company named Atsena Therapeutics has a gene therapy candidate (ATSN-201) that has received special designations from the FDA to expedite its development and review.Researchers are also working to:
While challenges remain, the progress in gene therapy and other research areas offers significant hope for future treatments that could slow, stop, or even reverse vision loss from XLRS.
References
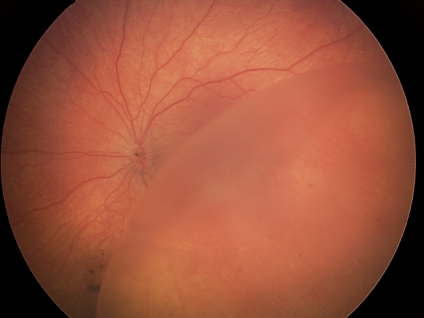
The characteristic schisis cavity or “bulla” is seen in the lower right-hand side of this retinal image.